What is trigeminal neuralgia?
Trigeminal neuralgia is a painful disorder of one of the nerves in your face, the trigeminal nerve
Cause
The precise cause of trigeminal neuralgia is unknown.
Experts think that it may be due to overstimulation of the trigeminal nerve, but in most cases, it is not known what causes this overstimulation.
The most common cause is thought to be a blood vessel pressing on the nerve.
In some cases, the cause may be a tumour, an inflammation (as in Multiple Sclerosis) or Postherpetic Trigeminal Neuralgia
Signs and symptoms
Trigeminal neuralgia occurs more often in women than in men and mostly seen in people over 40.
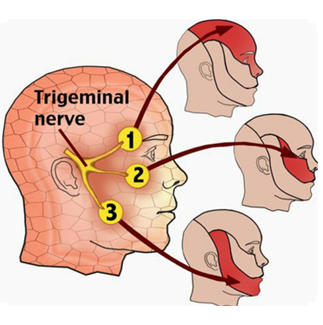
Patients with trigeminal neuralgia suffer brief but very severe stabbing pains in a particular part of their face, often near a corner of the mouth or a nostril.
Patients sometimes describe the pain as being like an electric shock, or like a stab with a hot needle.
The pains can be triggered by various stimuli or causes, such as wind blowing in one's face, washing, shaving, cold or heat, but also by chewing, speaking or swallowing.
Trigeminal neuralgia often leads to weight loss, as patients may be too afraid to eat. Some patients have specific sensitive sites ('trigger points') on their face where even a light touch may provoke a pain attack.
The complaints may be so serious that they seriously affect the patient's quality of life. The pains often occur over a particular period, after which they may disappear for a while.
Some patients only have a few of these pain periods in their whole lifetime, while others have them far more often.
How is trigeminal neuralgia diagnosed?
The diagnosis is based on the pattern of the patient's symptoms.
Physical examination
Neurological Examination to exclude other possible causes of the pain.
Do I need additional examinations?
If you visit the clinic because of trigeminal neuralgia, you will always be given an MRI scan of the brain, to exclude other possible causes of the pain.
What are my treatment possibilities?
Physical Treatments
1. Medication
Pharmacological treatment:
In medication treatment, the first choice is carbamazepine and oxcarbamazepine. Carbamazepine has a pain reducing effect in 70% of patients.
Other medication, as yet without clinical evidence of efficacy, can be tried, such as gabapentine, pregabaline or Baclofen
2. Interventional Pain Treatments
RFTC
Neurosurgical OPERATION (MVD)
What is a Gasserian Ganglion block (RFTC)?
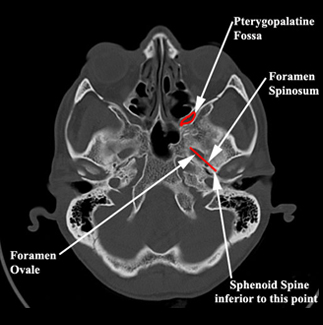
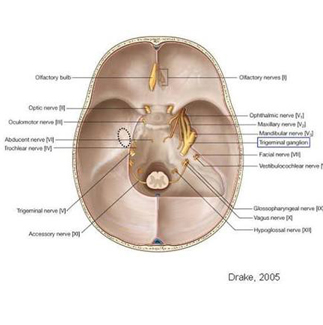
A ganglion is a bundle of interconnected nerves that are important for pain in a certain area of the body. One such ganglion is the Gasserian ganglion or trigeminal ganglion - this ganglion is important in the treatment of some types of facial pain.
It is possible to relieve pain by blocking the Gasserian ganglion. The Gasserian ganglion is found inside the skull next to the brainstem and has three nerve branches known as the trigeminal nerves. These three branches are responsible for sensation on one side of the face.
A block in one part of the Gasserian ganglion is achieved by applying electrical current to the Gasserian ganglion via a needle that heats the ganglion. This stops it from passing on any more pain signals.
Only the thin nerves in this ganglion are blocked. Since the thick nerves of the ganglion are not blocked, the remaining function of the ganglion remains intact. This Gasserian ganglion block is also known as the Sweet procedure.
When do I need a Sweet procedure?
Patients with classical facial pain, also named trigeminal neuralgia, are suitable for treatment with a Sweet procedure.
What should I be aware of before undergoing a Sweet procedure?
There are a number of situations that you should report your pain specialist if he proposes you a Sweet procedure:
In case of pregnancy you cannot undergo a Sweet procedure because X-ray equipment is used.
If you are ill or have fever on the day of treatment you cannot undergo a Sweet procedure and a new appointment has to be made.
If you are allergic to iodine, bandages, anaesthetics or contrast that you must notify your pain specialist before the appointment for the treatment is made.
If you take blood thinners you must notify that your pain specialist before the appointment for treatment is made. He will then consider certain medication advice to temporarily cease.
How should I prepare for a Sweet procedure?
No special preparations such as sleepwear are needed because the treatment is done on an outpatient basis.
You must not eat before your treatment and take your normal medication.
N.B.: this does not include blood thinners, as mentioned above.
Make sure you have someone to take you home, because you may not drive for 24 hours.
How does the Sweet procedure work?
The treatment will be performed in the surgical day-care centre, where you will be asked to change into a surgical gown.
A nurse will escort you to the treatment room, where there is a treatment table, an X-ray machine and television monitors.
You will be positioned on the treatment table on your back.
The blood pressure and the amount of oxygen in your blood will be controlled during the treatment.
An Intravenous line will be placed in your hand.
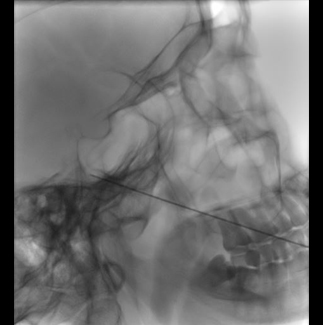
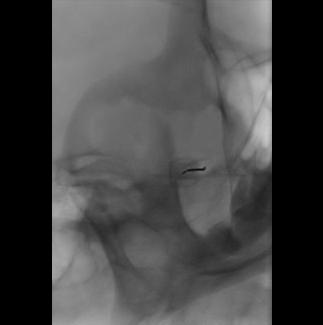
The right place of the block is estimated with aid of fluoroscopy
This place is marked on the skin with a felt pen.
The area around this site is then disinfected with a cold, betadine.
The pain specialist covers the area with sterile drapes.
Through the drip a small amount of short-lasting anaesthetic is injected, after which you will fall asleep.
If you wake up after a while, the pain specialist under fluoroscopy (via television monitor) has placed the needle in the correct position near the Gasserian ganglion.
Then small electrical currents are administrated near the Gasserian ganglion.
You will feel a tingling sensation in your face.
When you feel this, you must tell the treating pain specialist straight away, and not wait for it to become painful.
The pain specialist will ask you where you feel the sensation and you don't have to point the place with your finger.
By means of a special device, the pain specialist can read the distance from the needle to the ganglion. Is the needle in the right place you will be brought back to sleep again.
The pain specialist will give a radiofrequency (RF) electrical current via the needle to block the Gasserian ganglion.
Nowadays instead of a radiofrequency (RF) electrical current also a pulsed radiofrequency (PRF) electrical currents can be used to block the Gasserian ganglion.
The difference is that instead of one single radiofrequency electrical current an interrupted (pulsed) series of small electrical currents is used. These small currents produced less heat near the ganglion.
Less heat of the small currents does not lead to interruption of the ganglion but results more in modulation of the ganglion to decrease the pain.
After the treatment you have to stay at the day care centre for two hours or you will be hospitalised for 24 hrs.
After this treatment you need to make an appointment at the pain clinic after six to eight weeks with your own pain specialist. The effect of treatment will be checked and further policy will discuss with you.
What are dangers and side effects of a Sweet procedure?
After a Sweet procedure, the following complications or side effects can occur:
It is possible that small blood vessel can be hit by the needle resulting in haemorrhage of the cheek.
In rare cases a bacteria of the mucous membrane can enter the brain fluid resulting in meningitis.
If you develop a fever over 38.5 Co within 6 hours after the treatment together with headache and stiffness of the neck, you immediately have to contact the hospital or the pain clinic and you will be treated as soon as possible with antibiotics.
In case of repeated Sweet procedure numbness of a part of the face can remain. (Sensory loss in the treated branch)
Paralysis of the Masseter muscle
Anesthesia dolorosa
Corneal hypoesthesia and keratitis
Temporary paralysis of the third and fourth cranial nerves.
When can I expect pain relief after the treatment?
Afterpains can occur following a Sweet procedure. These may last for several weeks but will
Afterpains can occur following a Sweet procedure. These may last for several weeks but will eventually disappear.
The optimum results of treatment are seen after six to eight weeks.
Around this time, a new appointment with your pain specialist will be made.