Primary headaches
Secondary headaches
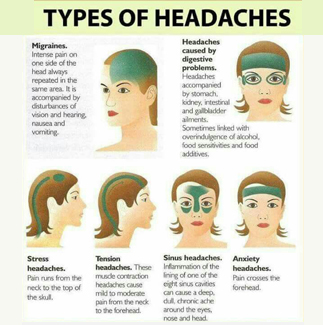
Migraine is a common disabling primary headache disorder
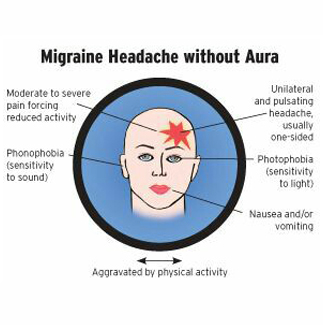
Migraine without aura is a clinical syndrome characterised by headache with specific features and associated symptoms. Migraine without aura is the commonest subtype of migraine. It has a higher average attack frequency and is usually more disabling than Migraine with aura. Migraine without aura often has a strict menstrual relationship. Migraine headache is usually frontotemporal.
DIAGNOSTIC CRITERIA
A. At least 5 attacks fulfilling criteria B-D
B. Headache attacks lasting 4-72 hours (untreated or unsuccessfully treated)
C. Headache has at least two of the following characteristics:
1. unilateral location
2. pulsating quality
3. moderate or severe pain intensity
4. aggravation by or causing avoidance of routine physical activity (eg, walking or climbing stairs)
D. During headache at least one of the following:
1. nausea and/or vomiting
2. photophobia and phonophobia
E. Not attributed to another disorder
When attacks occur on ≥15 days/month for >3 months, it is referred to as chronic migraine, provided there is no history of medication overuse
Migraine headache is commonly bilateral in young children; an adult pattern of unilateral pain usually emerges in late adolescence or early adult life.
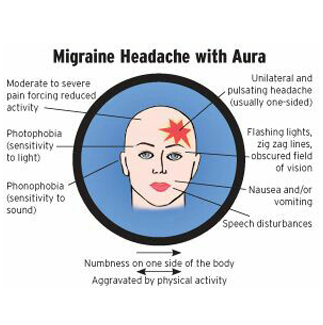
Migraine with aura is primarily characterised by the focal neurological symptoms that usually precede or sometimes accompany the headache. Some patients also experience a premonitory phase, occurring hours or days before the headache, and a headache resolution phase. Premonitory and resolution symptoms include hyperactivity, hypoactivity, depression, craving for particular foods, repetitive yawning and other less typical symptoms reported by some patients.
Recurrent disorder manifesting in attacks of reversible focal neurological symptoms that usually develop gradually over 5-20 minutes and last for less than 60 minutes. Headache with the features of migraine without aura usually follows the aura symptoms. Less commonly, headache lacks migrainous features or is completely absent.
Aggravating factors
Psychosocial stress, frequent intake of alcoholic beverages, other environmental factors.
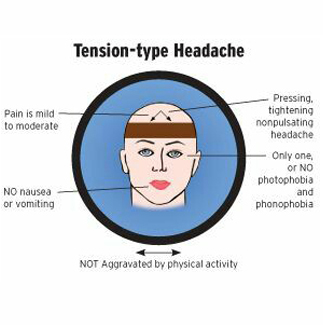
This is the most common type of primary headache
Diagnostic criteria for episodic tension type headache
A. At least 10 episodes occurring in 1 day a month on average (12 days a year) and fulfilling criteria B-D (infrequent episodic tension-type headache) or at least 10 episodes occurring on 1 but 15 days per month for at least three months (12 and 180 days per year) and fulfilling criteria B-D (frequent episodic tension-type headache)
C. Headache has at least two of the following characteristics:
1. bilateral location
2. pressing/tightening (non-pulsating) quality
3. mild or moderate intensity
4. not aggravated by routine physical activity such as walking or climbing stairs
D. Both of the following:
1. no nausea or vomiting (anorexia may occur)
2. no more than one of photophobia or phonophobia
E. Not attributed to another disorder
Chronic tension-type headache is less common, with a one-year prevalence of 2 3%. It typically evolves over time from episodic tension-type headache. It occurs, by definition, on more than 15 days a month, and may be daily.
The exact mechanism of tension-type headache is not known. Tension-type headache may be stress-related or associated with functional or structural cervical or cranial musculoskeletal abnormality.
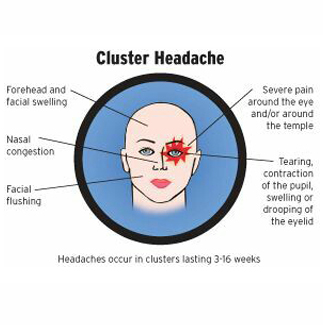
Trigeminal autonomic cephalalgias (TACs) are rare and are characterised by attacks of severe unilateral pain in a trigeminal distribution. They are associated with prominent ipsilateral cranial
autonomic features. Cluster headache (CH) is the most common TAC (estimated prevalence 1 in 1,000). Paroxysmal hemicrania (PH) is probably under-recognised (estimated prevalence 1 in 50,000). Short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT) and short-lasting unilateral neuralgiform headache attacks with cranial autonomic symptoms (SUNA) are very rare.
Attacks of severe, strictly unilateral pain which is orbital, supraorbital, temporal or in any combination of these sites, lasting 15-180 minutes and occurring from once every other day to 8 times a day. The attacks are associated with one or more of the following, all of which are ipsilateral: conjunctival injection, lacrimation, nasal congestion, rhinorrhoea, forehead and facial sweating, miosis, ptosis, eyelid oedema. Most patients are restless or agitated during an attack.
Age at onset is usually 20-40 years. For unknown reasons prevalence is 3-4 times higher in men than in women.
Diagnostic criteria
A. At least 5 attacks fulfilling criteria B-D
B. Severe or very severe unilateral orbital, supraorbital and/or temporal pain lasting 15-180 minutes if untreated
C. Headache is accompanied by at least one of the following:
D. Attacks have a frequency from one every other day to 8 per day
E. Not attributed to another disorder
Acute attacks involve activation of the posterior hypothalamic grey matter. Cluster headache may be inherited (autosomal dominant) in about 5% of cases. Attacks usually occur in series (cluster periods) lasting for weeks or months separated by remission periods usually lasting months or years. However, about 10-15% of patients have chronic symptoms without remissions.
During a cluster period, and in the chronic subtype, attacks occur regularly and may be provoked by alcohol, histamine or nitroglycerine. Pain is maximal orbitally, supraorbitally, temporally or in any combination of these sites, but may spread to other regions of the head. Pain almost invariably recurs on the same side during an individual cluster period. During the worst attacks, the intensity of pain is excruciating. Patients are usually unable to lie down and characteristically pace the floor.
Treatment of acute migraine
Pharmacological prophylaxis for migraine
Treatment of tension-type headache
Pharmacological prophylaxis for tension-type headaches
Acute treatment of cluster headaches
Pharmacological prophylaxis for cluster headaches