Causes of Cancer Pain
Most cancer pain is caused by the tumour pressing on bones, nerves or other organs in your body. Sometimes pain is related to your cancer treatment. For example, some chemotherapy drugs can cause numbness and tingling in your hands and feet or a burning sensation at the place where they are injected. Radiotherapy can cause skin redness and irritation.
Remember that some pain may have nothing to do with your cancer. You may have the general aches and pains that everyone gets from time to time.
Types of Cancer Pain
Cancer pain can be acute or chronic. Acute pain is due to damage caused by an injury and tends to only last a short time. For example, having an operation can cause acute pain. The pain goes when the wound heals. In the meantime, painkillers will usually keep it under control.
Chronic pain is pain caused by changes to nerves. Nerve changes may occur due to cancer pressing on nerves or due to chemicals produced by a tumour. It can also be caused by nerve changes due to cancer treatment. The pain continues long after the injury or treatment is over and can range from mild to severe. It can be there all the time and is also called persistent pain. Chronic pain can be difficult to treat, but painkillers or other pain control methods can successfully control it in about 95 out of every 100 people.
The amount of pain you have with cancer depends on
If you have pain it is very important to let your pain physician know straight away. If you try to put up with the pain, this can lead to nerve changes that may make the pain harder to control in the future
Cancer Pain Treatment
Oral Medications: Painkilling drugs work to control cancer pain in most people. The key to controlling cancer pain is to take your medicine on a regular schedule. Do not wait until your pain gets bad. Pain is easier to control when you treat it just after it starts.
Be careful when taking nonprescription medicines. Talk with a pain physician before you take these medicines, especially if you have a fever or have had kidney or liver disease, gastrointestinal bleeding, or a stomach ulcer. Prescription medicines may be used alone or with other medicines. Depending on your pain, some of these medicines work better than others. Prescription medicines include:
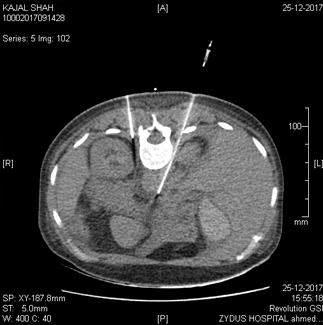
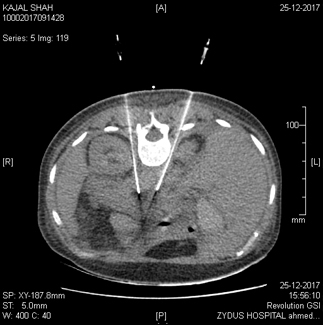
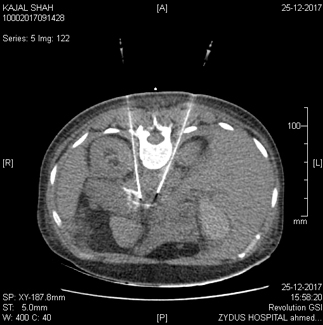
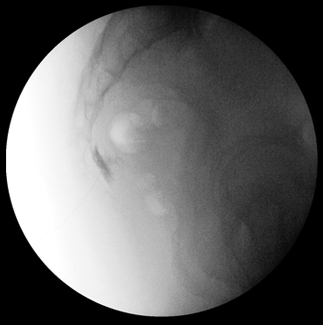
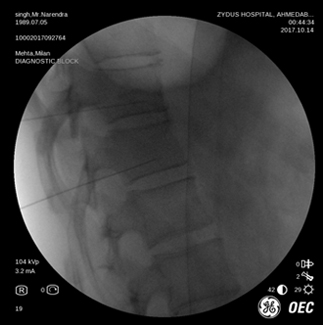
Nerve Blocks: Nerve blocks are injections containing potent anti-inflammatory agents directed at a particular nerve or nerve group that is intended to reduce inflammation and relieve pain.
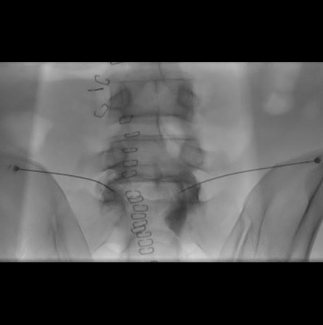
Intracthecal Pump: Also called infusion pain pumps or spinal drug delivery systems. In this procedure, a pocket is made under the skin that’s large enough to hold a medicine pump. The pump is usually about one inch thick and three inches wide. A catheter is also inserted, which carries pain medicine from the pump to the intrathecal space around the spinal cord. The
implants deliver medicines directly to the spinal cord, where pain signals travel. For this reason, intrathecal drug delivery can provide significant pain control with a fraction of the dose that would be required with pills. In addition, the system can cause fewer side effects than oral medications because less medicine is required to control pain.
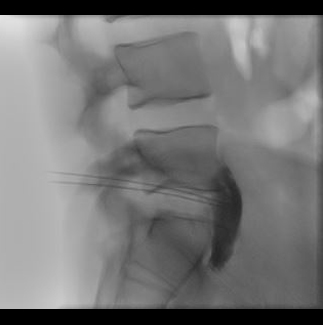
Radiofrequency Ablation: Radiofrequency ablation (or RFA) is a procedure used to reduce pain. An electrical current produced by a radio wave is used to heat up a small area of nerve tissue, thereby decreasing pain signals from that specific area. RFA can be used to help patients with chronic (long-lasting) cancer pain. RFA has proven to be a safe and effective way to treat some forms of pain. It also is generally well-tolerated, with very few associated complications.
Neurolytic Blocks
Neurolytic blocks refer to the blocks in which the target nerves are lysed (undergo change in structure) by injecting neurolytic agents. The commonly used neurolytic agents include absolute alcohol, phenol, glycerol. The neurolytic blocks are commonly given in cancer pain such as pancreatic cancer, bowel cancer, pelvic malignancy, oral cancer and non cancer pains such as trigeminal neuralgia. There is a chance of alcohol induced neuritis after administration of neurolytic blocks.
The common neurolytic blocks are as follows:
Mythe of Opioids
What are the myths about using opioids to treat cancer pain?
Many patients are reluctant to use opioids such as morphine, oxycodon, fentanyl, buprenorphine or methadon. These drugs should, of course, only be used in cases of severe pain and they do have side effects.
However, the fear of using opioids is very often based on prejudice or myths, such as:
1. Opioids are addictive!!
Not true: if you do not use more than you need to treat the pain, you will not become addicted.
2. Once you start using opioids, your days are over!!
Not true: strong painkillers are used to treat severe pain. If the pain decreases, for example, because treatment of the cancer is successful, you can reduce the morphine dosage in consultation with your doctor.
3. Using opioids means you have entered the final stage of a disease!!
Not true: morphine is simply a very effective painkiller that is used to treat severe pain, irrespective of the duration or severity of your disease.
4. It is best to take as few painkillers as possible!!
Not true: of course you should never use too many painkillers. But you should remember that pain can often be worse for you than painkillers.
5. Only take painkillers when you start to feel the pain!!
Not true: you should take painkillers at regular intervals in order to achieve basic pain relief. If you wait until the pain starts, you will be too late and will not achieve effective pain relief.
6. Opioids can cause apnoea!!
Not true: if you only take what painkillers are necessary to treat your pain, you will not suffer from apnoea.