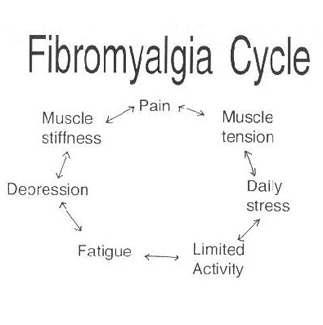
Fibromyalgia is a complex condition that is characterized by chronic widespread pain and multiple other symptoms, including fatigue, sleep disturbances, cognitive dysfunction, stiffness, and depressive episodes.
Fibromyalgia may coexist and/or overlap with other conditions that may involve central sensitivity, including chronic fatigue syndrome, irritable bowel syndrome, irritable bladder syndrome or interstitial cystitis, and temporomandibular disorder.
The pathophysiology of fibromyalgia remains uncertain but is believed to be partly the result of central systems affecting afferent processing as well as impaired endogenous pain inhibitory systems.
Fibromyalgia appears to have been identified in approximately 2% to 4% of the general population. Fibromyalgia is predominantly diagnosed in subjects between the ages of 20 and 60 years old, with approximately 80% of cases being female. Less cases of fibromyalgia being identified/diagnosed in men could be a function of a missed diagnosis.
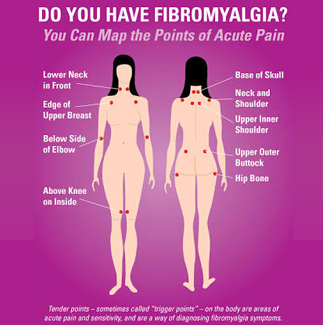
Fibromyalgia syndrome involves a constellation of symptoms, which may include chronic disseminated pain without synovitis, aches, and/or myofascial tenderness, fatigue, cognitive impairment, sleep disturbances (commonly alpha wave electroencephalographic anomaly), morning stiffness, prior disease and anxiety symptoms, impaired social occupational functioning, and sexual dysfunction.
The four most frequently described symptoms in clinical practice are:
ACR 2010 FIBROMYALGIA DIAGNOSTIC CRITERIA
A patient satisfies the diagnostic criteria for FMS if the following 3 conditions are met:
PATHOPHYSIOLOGY OF FIBROMYALGIA SYNDROME
Although the precise mechanisms contributing to the pathophysiology of
FMS remain to be fully elucidated, it is thought that
patients with fibromyalgia have impaired endogenous analgesic systems, in particular suboptimally functioning descending inhibitory pathways, which normally function to ameliorate pain as well as abnormal pain processing. These pathways are both serotonergic (eg, rostral ventral medulla) and noradrenergic (eg, dorsolateral pontine tegmentum), converging into the dorsal lateral funiculus, which synapse in rexed’s laminae I, II and V in the spinal cord dorsal horn. Abnormalities of sensitization in FMS may be seen in peripheral spinal and/or central supraspinal sites (central sensitization, neuroplasticity, hyperalgesia).
Evidence for genetic abnormalities in fibromyalgia has also been elucidated
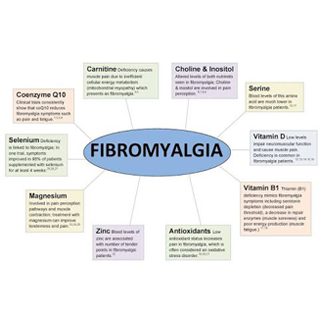
Serum ferritin levels were found to be significantly lower in FMS patients, perhaps due to the role of iron as a cofactor in enzymes involved in neurotransmitter synthesis.
Levels of magnesium and zinc were found to be low in some studies. Association between serum zinc level and number of tender points and between fatigue and magnesium level was also found to be meaningful.
Serum IL-8 levels were elevated in fibromyalgia patients as well, and these levels were reduced to near normal levels within 6 months after brief inpatient multidisciplinary pain therapy.
While studies attempting to localize the pathology in FMS to peripheral tissues have failed in showing any abnormalities in muscle tissue, Staud and coworkers did show that enhanced central pain processing can occur via continued peripheral muscle afferent input, Their study demonstrated that muscle lidocaine injections increased local pain thresholds and decreased remote secondary heat hyperalgesia in fibromyalgia patients, emphasizing the important role of peripheral impulse input in maintaining central sensitization.
Given the unclear etiology of fibromyalgia, and the heterogeneous presentations of the disease, it has become clear that no one therapy is broadly efficacious. The mainstay of management of fibromyalgia is graded exercise therapy, offered in conjunction with psychotherapeutic options to help equip patients with coping and pacing strategies, and relaxation techniques to help manage the pain better.
Non pharmacological treatments
TENS and acupuncture can help to some extent in managing the wide spread pain associated with fibromyalgia.
Pharmacological management
Anti neuropathic drugs have been shown to be efficacious in management of pain as well as sleep in fibromyalgia. These drugs include tricyclics, gabapentinoids and SNRI’s.
Psychotherapeutic options
Cognitive and behavioural therapy and relaxation techniques, offered as a part of multidisciplinary approach, can help in managing the pain better, with less dependence on drugs and health care professionals.
Interventional treatments for fibromyalgia
Patients who do not respond to conservative management may be offered injection treatment to facilitate a rehabilitative approach.
Trigger point injections
Trigger point injections with local anaesthetic and steroid can help in alleviating the myofascial pain associated with fibromyalgia.
Botox injections
Injection of botulinum toxin in to selective muscles can also help in alleviating the myofascial pain associated with fibromyalgia.